Tribalism, which is at the heart of so much human conflict — whether for cultural, religious, or racial reasons or simply greed and power — has been devastating for as long as modern humans have been around.
Such divisions are also common in other species, where, for example, quarrels leading to violence are common enough among chimpanzees and wherever species compete for resources such as water, food and territory.
Some version of tribalism plays out at the cellular level and never more so than in the immune system.
I used to think the nervous system was the most complex system in the body, but after struggling to bring myself up to date on the immune system in the wake of this year’s Nobel Prize in medicine, I’m not so sure.
The immune system is incredibly complex, too — intimidatingly so.
The challenge for the immune system is two-fold: mount effective responses to foreign invaders such as viruses and bacteria, while at the same time protecting the body’s cells from the same vigilant immune system.
The latter question and how it was solved was the subject of this year’s Nobel Prize in medicine and/or physiology.
The immune system begins with stem cells in the bone marrow, which mature in the thymus gland, a small organ located in the upper chest covered by the breastbone.
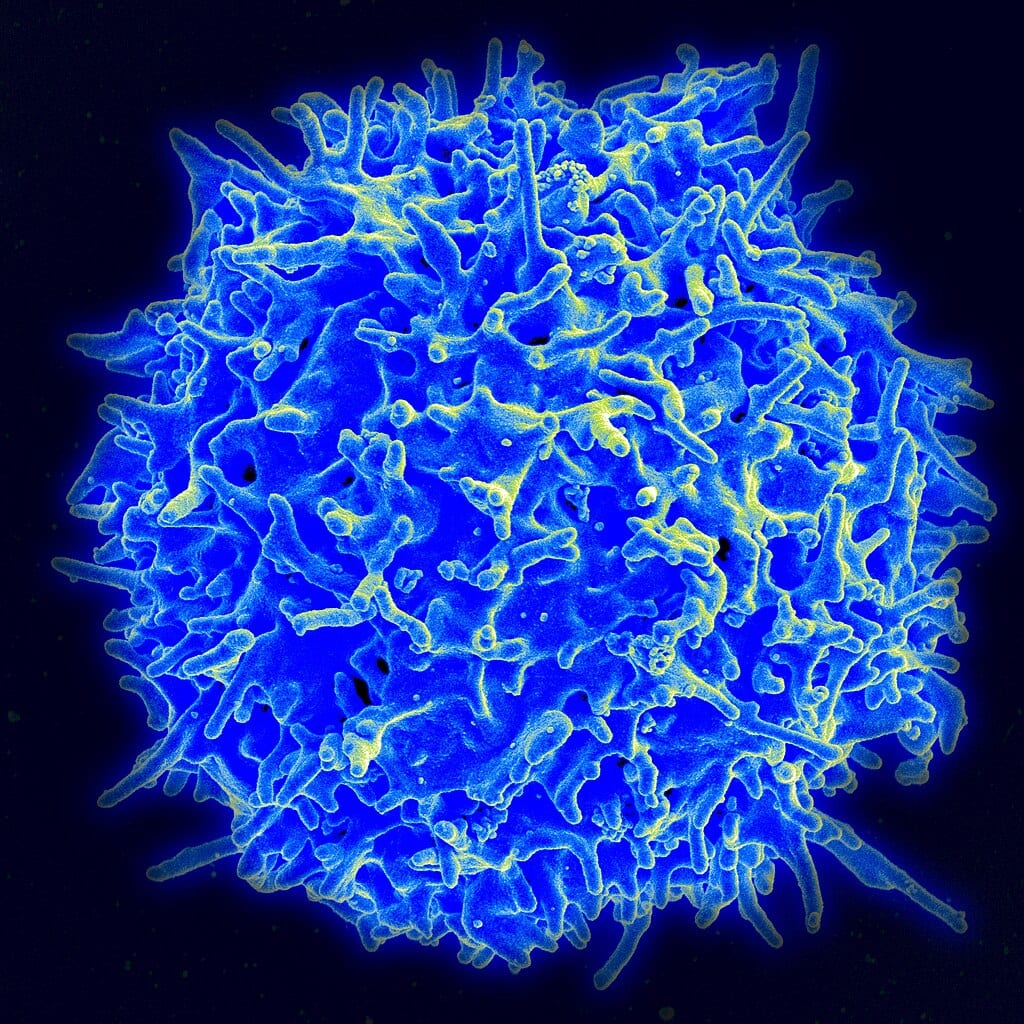
To protect against foreign invaders, cells in the thymus develop a myriad of lymphocytes (T cells), each T cell expressing a unique protein tag on its cell surface membrane, which, should it match a protein on the surface of a foreign invader such as a virus or other pathogen, sets in train a series of events to destroy the invader.
The system works surprisingly well and incorporates a memory for prior infections, the better to identify and attack like pathogens should subsequent attacks occur, such as COVID.
The system works but isn’t perfect, as some readers can no doubt attest, given that they may have had two or more attacks of COVID, despite timely vaccination with mRNA vaccines — themselves and their developers the subject of a Nobel Prize in 2023.
The thymus not only protects against foreign invaders but also identifies T cells which express “self” proteins on their surface, which might potentially trigger an attack on some of the body’s own cells, and marks them for destruction within the thymus.
It’s a marvellous “central” component to the immune system, but hardly perfect because some T cells that express “self” proteins on their surfaces manage to escape the thymus into the peripheral circulation, where they can provoke immune attacks on the body’s own cells — an autoimmune attack.
There had to be a second line of defence: a peripheral arm to the immune system to protect the body’s own cells, so reasoned Shimon Sakaguchi, an immunologist in Japan.
In the 1980s and 1990s, Sakaguchi discovered that injecting T cells from normal mice into mice whose thymus gland had been removed shortly after birth protected the recipients from the autoimmune attack provoked by thymectomy.
This suggested that injected T cells could function as “suppressor cells” to eliminate self-attacking cells.
Later, Sakaguchi demonstrated a subset of Suppressor T cells (CD4+CD25+) that seemed to be involved in regulating autoimmunity (now called T regulatory cells or Treg).
Other groups confirmed this part of the peripheral puzzle, but no one was sure what the mechanism behind it was.
Enter the other two laureates, Mary Brunkow and Fred Ramsdell, who set about identifying the exact mutant gene in the Scurfy mouse, an experimental model of a severe autoimmune disease.
This wasn’t easy in the 1990s — like “looking for a needle in a haystack,” as the Nobel committee put it.
Nonetheless, they were able to doggedly track down the culprit mutant gene to the never-before-studied mutant version of the Foxp3 gene.
Brunkow and Ramsdell were able to demonstrate backwards and forwards that this was the real thing (all of the mutant mice showed this mutation, and producing transgenic mice with increasing copy numbers of the normal-wild-type Foxp3 gene showed progressive rescue of the autoimmune phenotype).
Shortly afterwards, Brunkow and Ramsdell showed that a severe human autoimmune disorder (IPEX) showed the same sort of mutation in the human homolog of the same gene.
Then, in 2003, Sakaguchi’s group and others showed that healthy versions of the Foxp3 gene were crucial to the function of the regulatory T cells they had previously discovered.
Everything lined up. There really is a peripheral component to immune tolerance, as Sakaguchi originally suggested in the 1980s — it’s not all up to the thymus, important though that organ is.
This is a very solid story of science at its best, expressed in the imagination and dogged persistence of the three laureates.
They laid a firm foundation for modern day immunology and opened the way to exploring entirely novel ways to treat autoimmune diseases such as multiple sclerosis more effectively and safely, Type 1 diabetes mellitus, Crohn’s disease, ulcerative colitis as well as creating new avenues for preventing rejection of organ transplants, treating cancer and allergies such as the all too common and dangerous peanut allergy.
Congratulations to the laureates and the insight and wisdom of the Nobel committee in choosing to highlight this subject in a very complicated field, of which I’ve barely hinted in this essay and learned so much in the process.
Dr. William Brown is a professor of neurology at McMaster University and co-founder of the InfoHealth series at the Niagara-on-the-Lake Public Library.