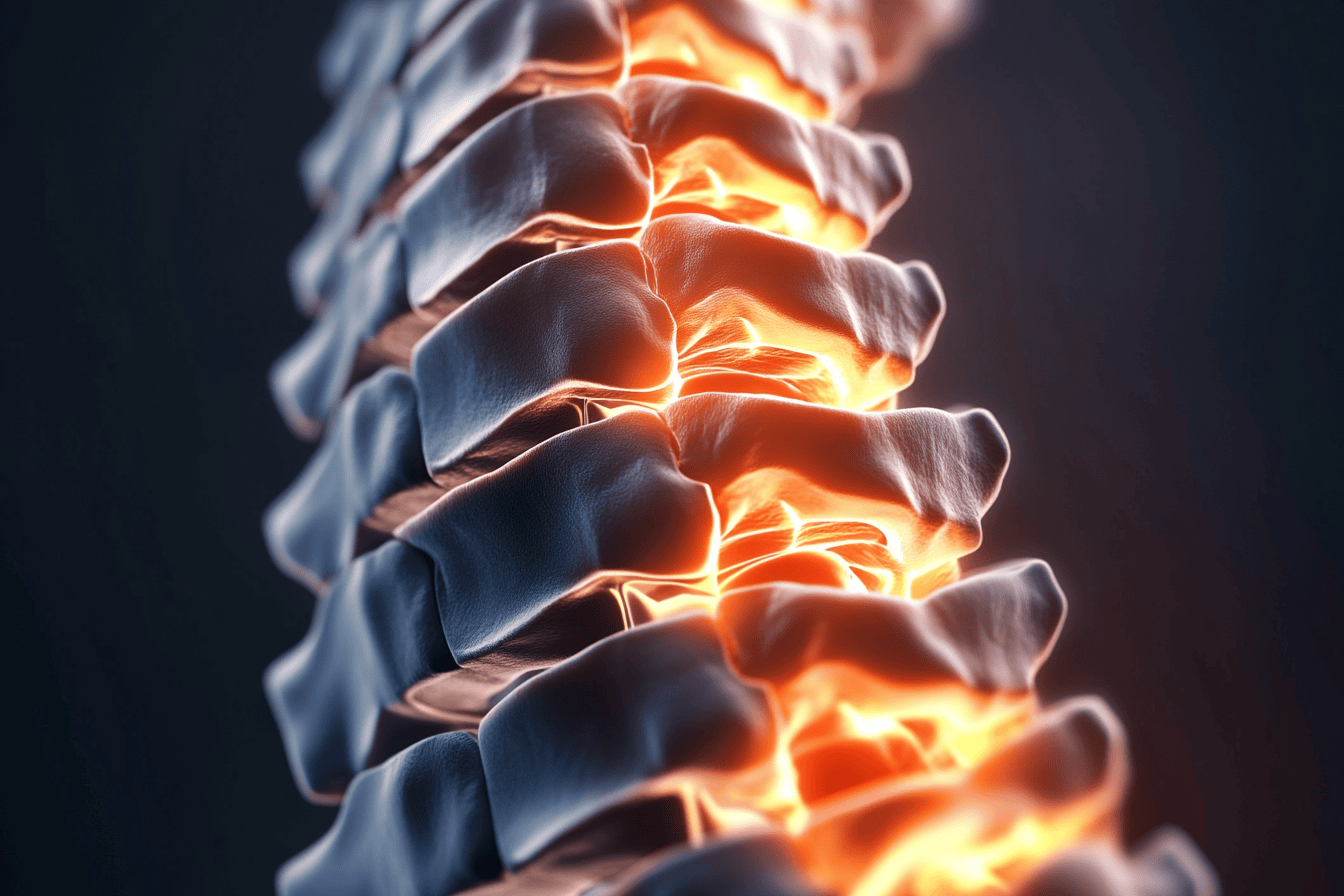
Low back and often leg pain in humans are common much past 50 years of age. The origins of lower back and neck problems are probably rooted in the evolution of bipedalism several million years ago, with our ancient ancestors in Africa. Bipedalism conferred enormous advantages but came at some cost. How so?
Getting about on the hindlimbs freed the forelimbs for fashioning and using tools, signaling to others and wielding weapons.
The cost was that compared to four-legged animals, the adoption of an erect posture, greatly increased the curvature and pressures in the neck and lower spine and in fully bipedal species who lived long enough, led to age-related wear and tear changes in the vertebrae, intervertebral discs, posterior joints and related ligaments in both the neck and lower back.
This essay focuses on the lower back and next week’s essay on the neck.
Much past 50 years of age, imaging studies in humans commonly reveal degenerative changes and compression of the vertebrae in the lumbosacral region, narrowed disc spaces between vertebrae, bulging discs and degenerative changes in posterior joints, which taken together can crowd the space through which the lower lumbar and upper sacral nerve roots must pass to reach the pelvis to form the lumbosacral plexus and the sciatic nerve (more on last in part three of this series).
Early on, those degenerative changes in the lumbosacral spine are usually asymptomatic but may become associated with chronic, often disabling pain in the lower back.
In some instances, the pain may be acute and severe in the lower back and one or both legs and accompanied by tingling and numbness in the legs.
Trying to sort out the precise cause of back and leg pain can be challenging, especially in later life, because the degenerative changes usually involve two or more levels in the lower back, such as L3-4, and especially the L4-L5 and L5-S1 levels.
The diagnostic importance of the location of the pain in the back and buttocks isn’t nearly as helpful as the location of the pain and especially tingling and numbness in the leg(s) for sorting out the cause of the symptoms.
For example, symptomatic L5 root lesions characteristically produce pain in the lateral buttock and lateral calf, tingling and numbness in the top of the foot, especially the big toe and possibly, and may be associated with weakness in dorsiflexion and eversion of the foot.
On the other hand, lesions which involve the S1 root are usually associated with pain extending into posterior buttock and back of the calf, tingling and/or numbness in the lateral side of the foot and toes and possibly weakness of the posterior calf muscles as well as a reduced or absent tendon reflex at the ankle.
Sorting out and managing the cause of lower back and leg pain is younger patients is usually easier because the symptoms, clinical findings and imaging studies usually agree and point unambiguously to a single level — the L4-L5 or L5-S1 level where a herniated or broken off piece of disc can usually be seen compressing the symptomatic root L5 or S1 root in a manner consistent with the clinical symptoms and findings.
Those are usually the easy cases to sort out.
The conundrum in later life is that degenerative changes in the lumbosacral spine often involve two or more levels in the lumbosacral spine.
In such cases, sorting out which clinical, radiological and electrodiagnostic features best explain the symptoms can be very challenging, even in the hands of experts, and the reason why surgery to relieve symptoms related to degenerative disease so often fails to relieve symptoms — and may even compound them.
That’s why specialty clinics that combine the expertise and perspectives of neurologists, neurosurgeons, orthopedic surgeons, rehabilitative medicine specialists, radiologists and physiotherapists are vital for assessing patients with low back and leg symptoms related to degenerative disease for coming up with plausible strategies for non-surgical and sometimes surgical treatment of patients with disabling back and leg pain.
Managing lower back and leg pain much past the age of 60 years of age can be tricky.
Figuring out what to do very much depends on the basics: Thorough histories and physical examinations, appropriate imaging studies read by experienced radiologists and overall assessments by surgical and medical specialists with lots of experience.
Together, they go a long way to providing the information patients need to understand what’s going on in their back and the pros and cons of options for medical and surgical management needed to make the best decisions, especially in complicated cases.
Fortunately, in recent years, controlled studies comparing non-surgical and surgical management have been carried out, which provide useful guidance when the team is trying to make the decision about management in consultation with the patient.
Those studies aren’t perfect for the obvious reason that, unlike most drug trials, it’s impossible to “blind” surgery and the placebo effect plays a part in colouring the results.
Even so, the discipline of rigorously assessing patients from the perspectives of different skill sets and perspectives helps patients reach better informed decisions in the imperfect world of managing chronic lower back pain.
Readers might be interested to learn that one of the best papers on surgery versus conservative care was reported in the New England Journal of Medicine (one of the top five medical journals in the world) by a team from London Health Sciences Centre, in London, Ont., published 2020.
Look for programs on these issues on April 2 and 9 at 2 p.m. at the NOTL Public Library.
Dr. William Brown is a professor of neurology at McMaster University and co-founder of the InfoHealth series at the Niagara-on-the-Lake Public Library.