Dr. William Brown is a professor of neurology at McMaster University and co-founder of the Infohealth series at the Niagara-on-the-Lake Public Library.
Dr. William Brown
Special to The Lake Report
In the early 1970s when I was a young staff neurologist in the department of clinical neurological sciences in London, Ont., our tool kit for studying the nervous system was limited to the clinical history and examination, lumbar puncture, plain X-rays, arteriograms, contrast myelography, electroencephalograms (EEGs), electromyograms (EMGs), radioisotope brain scans and an occasional air study.
Of those, the most useful tools were the clinical history and physical examination, which in skilled and experienced hands, were capable of localizing most lesions based on the time, course and nature of the symptoms and the clinical findings.
In those days neurosurgeons had the added practical advantage of confronting many of the diseases they managed in the operating room, where they could see what was going on, even if, as was so often the case, there wasn’t much to do for many of the problems they faced.
Neurologists and neurosurgeons learned from one another and radiologists and pathologists by presenting clinical cases and critically reviewing the history, clinical findings, course of the disease, any relevant laboratory findings, imaging studies, biopsy material or, if the patient unfortunately died, the findings at autopsy.
These days, imaging studies and other data often provide the answer, but not always. Clinical-pathological conferences still play an important role in educating physicians and keeping them up to date. In the United States, the New England Journal of Medicine weekly publishes “Case records of the Massachusetts General Hospital,” many of which cases are solved and manageable in life. I’ve found them a marvellous way to keep up to date and plan to incorporate some of that material in our continuing series about the brain at the NOTL library.
Beginning in the 1970s, there were several revolutions in imaging. First on the scene was computed X-ray tomography (CT scanning) which harnessed a computer to analyze focused X-ray beams as they rotated about the head to create virtual slices of the brain in three planes.
The results were amazing. For the first time we could see the grey matter of the neocortex and deeper nuclei and the vast web of connecting white matter. And with the aid of contrast agents, it was possible to see most tumours and even clots plugging arteries and veins.
Since then the resolution with CT scanning has improved and unlike MRIs, CT scans provide excellent resolution of bony structures.
But by far the greatest revolution came with the introduction of MRI (magnetic resonance imaging) technologies. MRI depends on the fact that in a strong magnetic field, protons in water molecules, tend to line up. If a brief radio frequency (RF) pulse is then applied, those protons are briefly thrown out of alignment and energized, after which the acquired energy decays.
The rate of decay of the energy released by the protons may then be converted by a computer into images that reflect differences in the water content of the underlying brain – more water proportionally in grey matter and less in white matter where there is more lipid and less water.
The result of all that technical magic is marvellous images of the brain in the three cardinal planes. By changing the frequency, strength and duration of the RF signal, and the strength of the magnetic field, different images may be created depending on the water content of the underlying brain.
For example, in the case of ischemic strokes, there are usually three types of tissue (healthy brain, brain at risk because of a marginal blood supply and dead brain), which can be differentiated from one another by diffusion/perfusion MRI scanning techniques.
The latter provide potentially brain-saving information about which areas of the brain are threatened and hence potentially salvageable if the circulation to them is restored in a timely fashion by dissolving the clot. Or in the case of a large artery, such as the middle cerebral artery, by physically extracting the clot through an intra-arterial catheter threaded up to the site of the clot.
MRI has also been adapted to create images that reflect local changes in oxygen consumption and blood flow that accompany specific tasks. Called functional MRI (fMRI) this tool has become the darling of psychologists and physiologists because it provides a useful tool for studying the localization of function in the brain in real time.
For example, tapping a finger, lights up the associated area in the motor cortex for controlling that finger, or in other examples, different areas of the brain light up in response to reading, hearing and speaking words or recognition of familiar faces or perhaps remembering a favourite driving or walking route.
Perhaps most dramatic was the finding in severely brain injured patients who were wakeful but unable to respond, that when they were asked to imagine walking through a familiar neighbourhood or through their home, their brains lit up in the same areas as healthy subjects given the same instructions.
Those findings strongly suggested that some patients, thought to be functionally brain dead, understand and process information in the same places as you and I, yet are unable to show us that they understand.
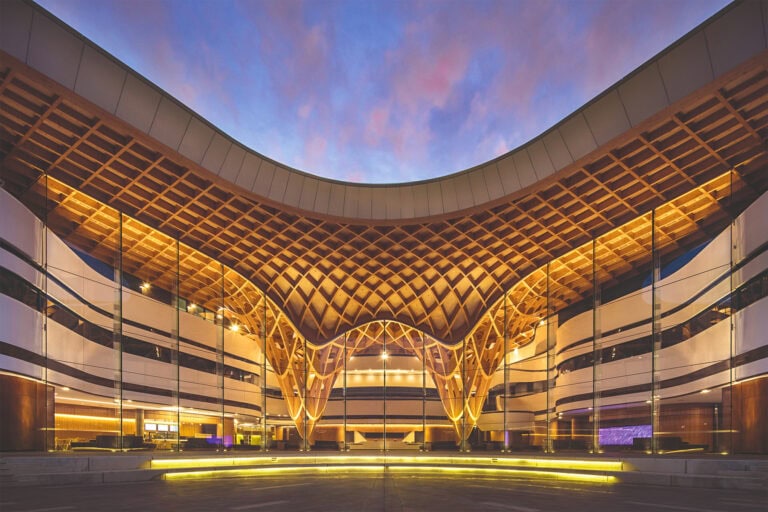
These and other promising technologies such as genetics and computer-assisted brain recording and stimulation technologies are the subject of the second and third sessions in the BRAIN series on March 10 and 17 at 2 p.m. using zoom through the NOTL library.